38.2: Mfupa
- Page ID
- 175523
Ujuzi wa Kuendeleza
- Kuainisha aina tofauti za mifupa katika mifupa
- Eleza jukumu la aina tofauti za seli katika mfupa
- Eleza jinsi mfupa huunda wakati wa maendeleo
Mfupa, au tishu za osseous, ni tishu zinazojumuisha ambazo hufanya endoskeleton. Ina seli maalumu na tumbo la chumvi za madini na nyuzi za collagen.
Chumvi za madini hasa ni pamoja na hydroxyapatite, madini yaliyotokana na phosphate ya kalsiamu. Calcification ni mchakato wa uhifadhi wa chumvi za madini kwenye tumbo la nyuzi za collagen ambayo huangaza na kuimarisha tishu. Mchakato wa calcification hutokea tu mbele ya nyuzi za collagen.
Mifupa ya mifupa ya binadamu huwekwa kwa sura yao: mifupa ndefu, mifupa mafupi, mifupa ya gorofa, mifupa ya sutural, mifupa ya sesamoid, na mifupa ya kawaida (Kielelezo\(\PageIndex{1}\)).
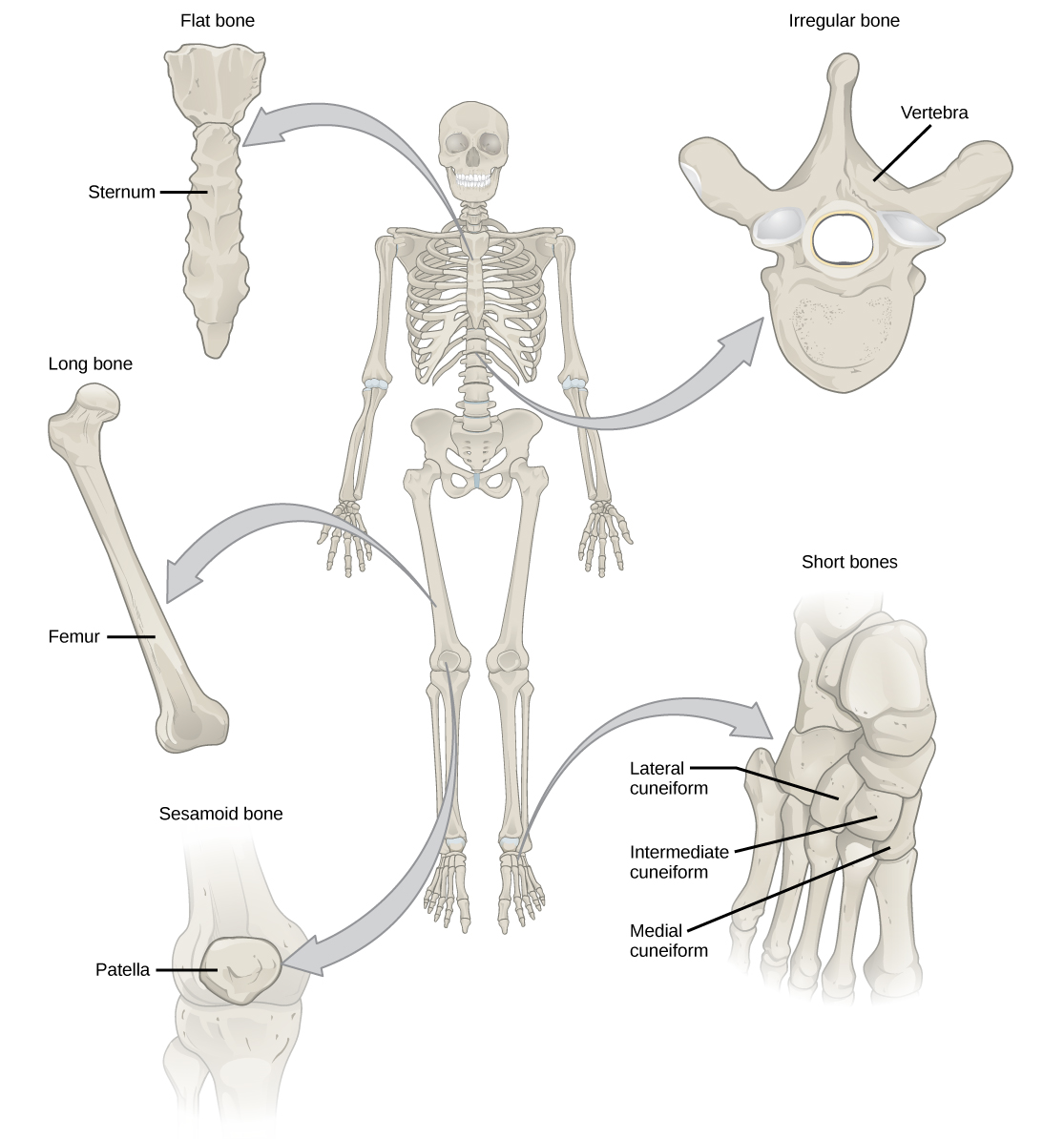
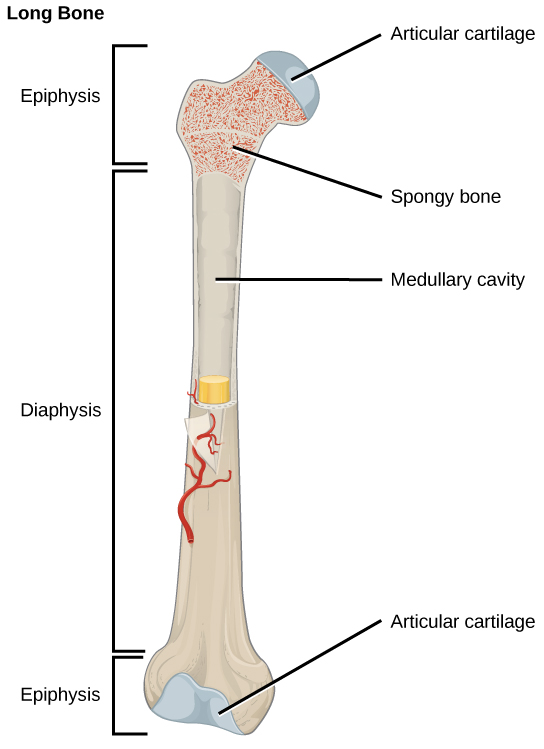
Mifupa mirefu ni mirefu kuliko ilivyo pana na ina shimoni na ncha mbili. Diaphysis, au shimoni kuu, ina mchanga wa mfupa katika cavity ya mchanga. Mwisho wa mviringo, epiphyses, hufunikwa na cartilage ya articular na hujazwa na marongo nyekundu ya mfupa, ambayo hutoa seli za damu (Kielelezo\(\PageIndex{2}\)). Wengi wa mifupa ya kiungo ni mifupa marefu- kwa mfano, femur, tibia, ulna, na radius. Tofauti na hii ni pamoja na patella na mifupa ya mkono na mguu.
Mifupa mafupi, au mifupa ya cuboidal, ni mifupa ambayo ni upana na urefu sawa, na kuwapa sura kama mchemraba. Kwa mfano, mifupa ya mkono (carpals) na mguu (tarsals) ni mifupa mafupi (Kielelezo\(\PageIndex{1}\)).
Mifupa ya gorofa ni mifupa nyembamba na mpana kiasi ambayo hupatikana ambapo ulinzi mkubwa wa viungo unahitajika au ambapo nyuso pana za attachment misuli zinahitajika. Mifano ya mifupa ya gorofa ni sternum (mfupa wa kifua), mbavu, scapulae (vile vya bega), na paa la fuvu (Kielelezo\(\PageIndex{1}\)).
Mifupa isiyo ya kawaida ni mifupa yenye maumbo magumu. Mifupa haya yanaweza kuwa na nyuso fupi, za gorofa, zisizochapishwa, au zilizopigwa. Mifano ya mifupa ya kawaida ni vertebrae, mifupa ya hip, na mifupa kadhaa ya fuvu.
Mifupa ya sesamoidi ni ndogo, mifupa bapa na huumbwa sawa na mbegu ya ufuta. Patellae ni mifupa ya sesamoid (Kielelezo\(\PageIndex{3}\)). Mifupa ya Sesamoid huendeleza ndani ya tendons na inaweza kupatikana karibu na viungo kwenye magoti, mikono, na miguu.

Mifupa ya sutural ni ndogo, gorofa, mifupa isiyo ya kawaida. Zinaweza kupatikana kati ya mifupa ya gorofa ya fuvu. Zinatofautiana katika idadi, sura, ukubwa, na nafasi.
Tissue mfupa
Mifupa huchukuliwa viungo kwa sababu yana aina mbalimbali za tishu, kama vile damu, tishu zinazojumuisha, neva, na tishu za mfupa. Osteocytes, seli hai za tishu mfupa, huunda tumbo la madini ya mifupa. Kuna aina mbili za tishu mfupa: compact na spongy.
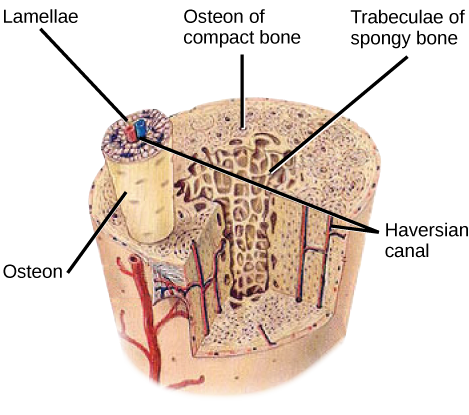
Compact mfupa tishu
Mfupa mzuri (au mfupa wa kamba) huunda safu ya nje ya mifupa yote na huzunguka cavity ya medullary, au mchanga wa mfupa. Inatoa ulinzi na nguvu kwa mifupa. Tissue mfupa thabiti ina vitengo vinavyoitwa osteons au mifumo ya Haversian. Osteons ni miundo ya cylindrical ambayo ina matrix ya madini na osteocytes hai iliyounganishwa na canaliculi, ambayo husafirisha damu. Wao ni iliyokaa sawa na mhimili mrefu wa mfupa. Kila osteon ina lamellae, ambayo ni tabaka za tumbo la compact inayozunguka mfereji wa kati unaoitwa mfereji wa Haversian. Mfereji wa Haversian (mfereji wa osteonic) una mishipa ya damu ya mfupa na nyuzi za neva (Kielelezo\(\PageIndex{4}\)). Osteons katika tishu mfupa compact ni iliyokaa katika mwelekeo huo pamoja na mistari ya dhiki na kusaidia mfupa kupinga bending au fracturing. Kwa hiyo, tishu za mfupa za kompakt ni maarufu katika maeneo ya mfupa ambayo inasisitiza hutumiwa kwa njia chache tu.
Sanaa Connection
Ni ipi kati ya taarifa zifuatazo kuhusu tishu za mfupa ni uongo?
- Tissue mfupa thabiti ni ya osteons cylindrical kwamba ni iliyokaa kama kwamba wao kusafiri urefu wa mfupa.
- Mifereji ya Haversian ina mishipa ya damu tu.
- Mifereji ya Haversian ina mishipa ya damu na nyuzi za neva.
- Tissue ya spongy hupatikana kwenye mambo ya ndani ya mfupa, na tishu za mfupa za mfupa hupatikana kwenye nje.
Tissue ya mfupa wa spongy
Wakati kompakt mfupa tishu aina safu ya nje ya mifupa yote, spongy mfupa au cancellous mfupa aina safu ya ndani ya mifupa yote. Tissue ya mfupa ya spongy haina osteons ambayo hufanya tishu za mfupa. Badala yake, lina trabeculae, ambayo ni lamellae ambayo hupangwa kama fimbo au sahani. Uboho mweusi wa mfupa hupatikana kati ya trabuculae. Mishipa ya damu ndani ya tishu hii hutoa virutubisho kwa osteocytes na kuondoa taka. Mafuta nyekundu ya mfupa wa femur na mambo ya ndani ya mifupa mengine makubwa, kama vile ileum, huunda seli za damu.
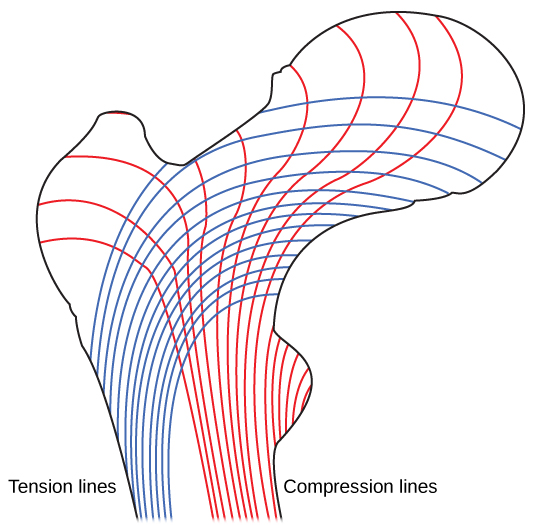
Mfupa wa spongy hupunguza wiani wa mfupa na inaruhusu mwisho wa mifupa ndefu kuimarisha kama matokeo ya matatizo yaliyotumika kwenye mfupa. Mfupa wa spongy ni maarufu katika maeneo ya mifupa ambayo hayajasisitizwa sana au ambapo matatizo yanafika kutoka pande nyingi. Epiphyses ya mifupa, kama shingo ya femur, inakabiliwa na shida kutoka kwa njia nyingi. Fikiria kuwekewa picha nzito iliyowekwa gorofa kwenye sakafu. Unaweza kushikilia upande mmoja wa picha na dawa ya meno ikiwa dawa ya meno ilikuwa perpendicular kwa sakafu na picha. Sasa kuchimba shimo na fimbo toothpick ndani ya ukuta ili kunyongwa picha. Katika kesi hiyo, kazi ya dawa ya meno ni kusambaza shinikizo la chini la picha kwenye ukuta. Nguvu kwenye picha ni moja kwa moja chini ya sakafu, lakini nguvu kwenye dawa ya meno ni waya wa picha unaovuta chini na chini ya shimo kwenye ukuta unasumaji. Dawa ya meno itavunja haki kwenye ukuta.
Shingo la femur ni usawa kama dawa ya meno katika ukuta. Uzito wa mwili unasuuza chini karibu na ushirikiano, lakini diaphysis ya wima ya femur inasubu kwa upande mwingine. Shingo la femur lazima iwe na nguvu ya kutosha kuhamisha nguvu ya chini ya uzito wa mwili kwa usawa na shimoni la wima la femur (Kielelezo\(\PageIndex{5}\)).
Aina ya seli katika Mifupa
Mfupa una aina nne za seli: osteoblasts, osteoclasts, osteocytes, na seli za osteoprogenitor. Osteoblasts ni seli za mfupa zinazohusika na malezi ya mfupa. Osteoblasts kuunganisha na secrete sehemu ya kikaboni na sehemu isokaboni ya tumbo extracellular ya tishu mfupa, na collagen nyuzi. Osteoblasts hupigwa katika secretions hizi na kutofautisha katika osteocytes chini ya kazi. Osteoclasts ni seli kubwa za mfupa zilizo na nuclei 50. Wanaondoa muundo wa mfupa kwa kutolewa kwa enzymes za lysosomal na asidi zinazofuta tumbo la bony. Madini haya, iliyotolewa kutoka mifupa ndani ya damu, kusaidia kudhibiti viwango vya kalsiamu katika maji ya mwili. Mfupa pia unaweza kurejeshwa kwa ajili ya kurekebisha, ikiwa matatizo yaliyotumika yamebadilika. Osteocytes ni seli za mfupa zilizokomaa na ni seli kuu katika tishu zinazojumuisha bony; seli hizi haziwezi kugawa. Osteocytes huhifadhi muundo wa kawaida wa mfupa kwa kuchakata chumvi za madini katika tumbo la bony. Seli za osteoprogenitor ni seli za shina za squamous zinazogawanyika kuzalisha seli za binti zinazotofautisha katika osteoblasts Siri za Osteoprogenitor ni muhimu katika ukarabati wa fractures.
Maendeleo ya Mfupa
Ossification, au osteogenesis, ni mchakato wa malezi ya mfupa na osteoblasts. Ossification ni tofauti na mchakato wa calcification; wakati calcification hufanyika wakati wa ossification ya mifupa, inaweza pia kutokea katika tishu nyingine. Ossification huanza takriban wiki sita baada ya mbolea katika kiinitete. Kabla ya wakati huu, mifupa ya embryonic ina kabisa ya utando wa nyuzi na cartilage ya hyaline. Maendeleo ya mfupa kutoka kwenye membrane ya nyuzi huitwa ossification ya intramembranous; maendeleo kutoka kwa cartilage ya hyaline inaitwa ossification endochondral. Ukuaji wa mifupa unaendelea hadi takriban umri 25. Mifupa inaweza kukua kwa unene katika maisha yote, lakini baada ya umri wa miaka 25, ossification hufanya kazi hasa katika ukarabati wa mfupa na ukarabati.
Intramembranous Ossification
Ossification ya ndani ni mchakato wa maendeleo ya mfupa kutoka kwa membrane ya nyuzi. Inashiriki katika malezi ya mifupa ya gorofa ya fuvu, mandible, na clavicles. Ossification huanza kama seli za mesenchymal zinaunda template ya mfupa wa baadaye. Wao hufautisha katika osteoblasts kwenye kituo cha ossification. Osteoblasts hutoa tumbo la ziada na kalsiamu ya amana, ambayo huzidisha tumbo. Sehemu isiyo ya madini ya mfupa au osteoid inaendelea kuunda karibu na mishipa ya damu, na kutengeneza mfupa wa spongy. Tissue zinazojumuisha katika tumbo hufafanua katika mchanga mwembamba wa mfupa katika fetusi. Mfupa wa spongy hurejeshwa kwenye safu nyembamba ya mfupa wa compact juu ya uso wa mfupa wa spongy.
Endochondral Ossification
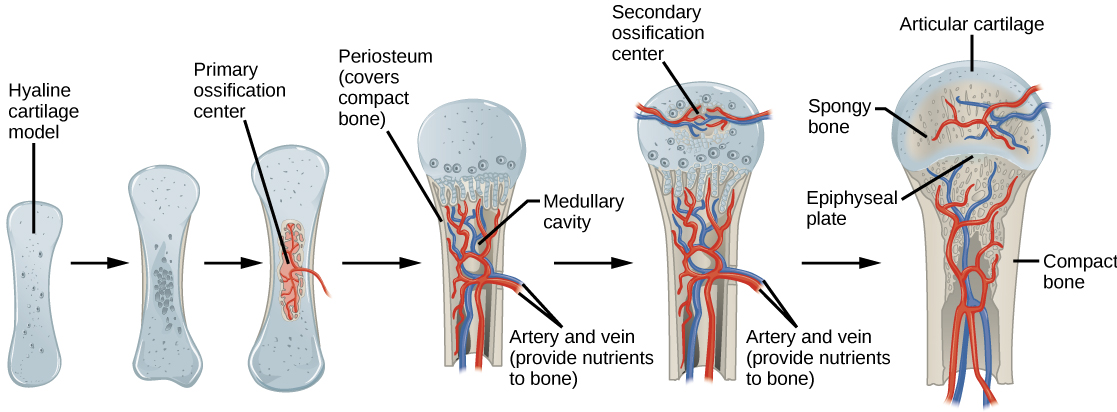
Ossification ya Endochondral ni mchakato wa maendeleo ya mfupa kutoka kwa cartilage ya hyaline. Mifupa yote ya mwili, isipokuwa kwa mifupa ya gorofa ya fuvu, mandible, na clavicles, hutengenezwa kwa njia ya ossification endochondral.
Katika mifupa ndefu, chondrocytes huunda template ya diaphysis ya hyaline cartilage. Kujibu ishara tata za maendeleo, tumbo huanza kuhesabu. Calcification hii inazuia kuenea kwa virutubisho ndani ya tumbo, na kusababisha chondrocytes kufa na ufunguzi wa cavities katika cartilage ya diaphysis. Mishipa ya damu huvamia cavities, na osteoblasts na osteoclasts kurekebisha calcified cartilage tumbo katika mfupa spongy. Osteoclasts kisha kuvunja baadhi ya mfupa spongy kujenga uboho, au medullary, cavity katikati ya diaphysis. Tissue, isiyo ya kawaida ya kawaida huunda sheath (periosteum) karibu na mifupa. Periosteum husaidia katika kuunganisha mfupa kwa tishu zinazozunguka, tendons, na mishipa. Mfupa unaendelea kukua na kuenea kama seli za cartilage kwenye epiphyses zinagawanyika.
Katika hatua ya mwisho ya maendeleo ya mfupa kabla ya kujifungua, vituo vya epiphyses huanza kuhesabu. Vituo vya ossification vya sekondari vinaunda katika epiphyses kama mishipa ya damu na osteoblasts huingia maeneo haya na kubadilisha cartilage ya hyaline ndani ya mfupa wa spongy. Mpaka ujana, cartilage ya hyaline inaendelea kwenye sahani ya epiphyseal (sahani ya ukuaji), ambayo ni kanda kati ya diaphysis na epiphysis ambayo inawajibika kwa ukuaji wa mifupa ya muda mrefu (Kielelezo\(\PageIndex{6}\)).
Growth of Bone
Long bones continue to lengthen, potentially until adolescence, through the addition of bone tissue at the epiphyseal plate. They also increase in width through appositional growth.
Lengthening of Long Bones
Chondrocytes on the epiphyseal side of the epiphyseal plate divide; one cell remains undifferentiated near the epiphysis, and one cell moves toward the diaphysis. The cells, which are pushed from the epiphysis, mature and are destroyed by calcification. This process replaces cartilage with bone on the diaphyseal side of the plate, resulting in a lengthening of the bone.
Long bones stop growing at around the age of 18 in females and the age of 21 in males in a process called epiphyseal plate closure. During this process, cartilage cells stop dividing and all of the cartilage is replaced by bone. The epiphyseal plate fades, leaving a structure called the epiphyseal line or epiphyseal remnant, and the epiphysis and diaphysis fuse.
Thickening of Long Bones
Appositional growth is the increase in the diameter of bones by the addition of bony tissue at the surface of bones. Osteoblasts at the bone surface secrete bone matrix, and osteoclasts on the inner surface break down bone. The osteoblasts differentiate into osteocytes. A balance between these two processes allows the bone to thicken without becoming too heavy.
Bone Remodeling and Repair
Bone renewal continues after birth into adulthood. Bone remodeling is the replacement of old bone tissue by new bone tissue. It involves the processes of bone deposition by osteoblasts and bone resorption by osteoclasts. Normal bone growth requires vitamins D, C, and A, plus minerals such as calcium, phosphorous, and magnesium. Hormones such as parathyroid hormone, growth hormone, and calcitonin are also required for proper bone growth and maintenance.
Bone turnover rates are quite high, with five to seven percent of bone mass being recycled every week. Differences in turnover rate exist in different areas of the skeleton and in different areas of a bone. For example, the bone in the head of the femur may be fully replaced every six months, whereas the bone along the shaft is altered much more slowly.
Bone remodeling allows bones to adapt to stresses by becoming thicker and stronger when subjected to stress. Bones that are not subject to normal stress, for example when a limb is in a cast, will begin to lose mass. A fractured or broken bone undergoes repair through four stages:
- Blood vessels in the broken bone tear and hemorrhage, resulting in the formation of clotted blood, or a hematoma, at the site of the break. The severed blood vessels at the broken ends of the bone are sealed by the clotting process, and bone cells that are deprived of nutrients begin to die.
- Within days of the fracture, capillaries grow into the hematoma, and phagocytic cells begin to clear away the dead cells. Though fragments of the blood clot may remain, fibroblasts and osteoblasts enter the area and begin to reform bone. Fibroblasts produce collagen fibers that connect the broken bone ends, and osteoblasts start to form spongy bone. The repair tissue between the broken bone ends is called the fibrocartilaginous callus, as it is composed of both hyaline and fibrocartilage (Figure \(\PageIndex{7}\)). Some bone spicules may also appear at this point.
- The fibrocartilaginous callus is converted into a bony callus of spongy bone. It takes about two months for the broken bone ends to be firmly joined together after the fracture. This is similar to the endochondral formation of bone, as cartilage becomes ossified; osteoblasts, osteoclasts, and bone matrix are present.
- The bony callus is then remodelled by osteoclasts and osteoblasts, with excess material on the exterior of the bone and within the medullary cavity being removed. Compact bone is added to create bone tissue that is similar to the original, unbroken bone. This remodeling can take many months, and the bone may remain uneven for years.

Scientific Method Connection: Decalcification of Bones
Question: What effect does the removal of calcium and collagen have on bone structure?
Background: Conduct a literature search on the role of calcium and collagen in maintaining bone structure. Conduct a literature search on diseases in which bone structure is compromised.
Hypothesis: Develop a hypothesis that states predictions of the flexibility, strength, and mass of bones that have had the calcium and collagen components removed. Develop a hypothesis regarding the attempt to add calcium back to decalcified bones.
Test the hypothesis: Test the prediction by removing calcium from chicken bones by placing them in a jar of vinegar for seven days. Test the hypothesis regarding adding calcium back to decalcified bone by placing the decalcified chicken bones into a jar of water with calcium supplements added. Test the prediction by denaturing the collagen from the bones by baking them at 250°C for three hours.
Analyze the data: Create a table showing the changes in bone flexibility, strength, and mass in the three different environments.
Report the results: Under which conditions was the bone most flexible? Under which conditions was the bone the strongest?
Draw a conclusion: Did the results support or refute the hypothesis? How do the results observed in this experiment correspond to diseases that destroy bone tissue?
Summary
Bone, or osseous tissue, is connective tissue that includes specialized cells, mineral salts, and collagen fibers. The human skeleton can be divided into long bones, short bones, flat bones, and irregular bones. Compact bone tissue is composed of osteons and forms the external layer of all bones. Spongy bone tissue is composed of trabeculae and forms the inner part of all bones. Four types of cells compose bony tissue: osteocytes, osteoclasts, osteoprogenitor cells, and osteoblasts. Ossification is the process of bone formation by osteoblasts. Intramembranous ossification is the process of bone development from fibrous membranes. Endochondral ossification is the process of bone development from hyaline cartilage. Long bones lengthen as chondrocytes divide and secrete hyaline cartilage. Osteoblasts replace cartilage with bone. Appositional growth is the increase in the diameter of bones by the addition of bone tissue at the surface of bones. Bone remodeling involves the processes of bone deposition by osteoblasts and bone resorption by osteoclasts. Bone repair occurs in four stages and can take several months.
Art Exercise
Figure \(\PageIndex{4}\): Which of the following statements about bone tissue is false?
- Compact bone tissue is made of cylindrical osteons that are aligned such that they travel the length of the bone.
- Haversian canals contain blood vessels only.
- Haversian canals contain blood vessels and nerve fibers.
- Spongy tissue is found on the interior of the bone, and compact bone tissue is found on the exterior.
- Answer
-
B
Glossary
- appositional growth
- increase in the diameter of bones by the addition of bone tissue at the surface of bones
- bone
- (also, osseous tissue) connective tissue that constitutes the endoskeleton
- bone remodeling
- replacement of old bone tissue by new bone tissue
- calcification
- process of deposition of mineral salts in the collagen fiber matrix that crystallizes and hardens the tissue
- compact bone
- forms the hard external layer of all bones
- diaphysis
- central shaft of bone, contains bone marrow in a marrow cavity
- endochondral ossification
- process of bone development from hyaline cartilage
- epiphyseal plate
- region between the diaphysis and epiphysis that is responsible for the lengthwise growth of long bones
- epiphysis
- rounded end of bone, covered with articular cartilage and filled with red bone marrow, which produces blood cells
- flat bone
- thin and relatively broad bone found where extensive protection of organs is required or where broad surfaces of muscle attachment are required
- Haversian canal
- contains the bone’s blood vessels and nerve fibers
- intramembranous ossification
- process of bone development from fibrous membranes
- irregular bone
- bone with complex shapes; examples include vertebrae and hip bones
- lamella
- layer of compact tissue that surrounds a central canal called the Haversian canal
- long bone
- bone that is longer than wide, and has a shaft and two ends
- osteoblast
- bone cell responsible for bone formation
- osteoclast
- large bone cells with up to 50 nuclei, responsible for bone remodeling
- osteocyte
- mature bone cells and the main cell in bone tissue
- osseous tissue
- connective tissue that constitutes the endoskeleton
- ossification
- (also, osteogenesis) process of bone formation by osteoblasts
- osteon
- cylindrical structure aligned parallel to the long axis of the bone
- resorption
- process by which osteoclasts release minerals stored in bones
- sesamoid bone
- small, flat bone shaped like a sesame seed; develops inside tendons
- short bone
- bone that has the same width and length, giving it a cube-like shape
- spongy bone tissue
- forms the inner layer of all bones
- suture bone
- small, flat, irregularly shaped bone that forms between the flat bones of the cranium
- trabeculae
- lamellae that are arranged as rods or plates



